GENERAL MEDICINE CASE
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
December 19,2021
65 YEAR OLD MALE WITH FEVER UNDER EVALUATION.
65 year old male came to casualty with chief complaints of high grade fever with chills since 10 days.
History of present illness:
Patient was apparently asymptomatic 10 days back then he developed high grade fever with chills and backache.
Patient also had 3-4 episodes of vomitings since 5 days.
He also complaints of swellings of legs 2 day prior to the onset of fever which subsided without any treatment.
No complaints SOB,cough,burning micturition, and loose stools.
Patient's daily routine:-
Past history:-
Patient was diagnosed with DM 5 years ago started on OHA.
Currently patient is on INJ .MIXTARD 10 U in the morning & 8 U at night
4 years ago patient came to our hospital with c/o SOB and was told to have lung infection and ?mass and was started on insulin.
Since 4 years patient had skin lesions with scaling over legs and hands which progressed gradually,for which he used steroids and tapered.As the lesions kept progressing patient underwent skin biopsy 1month ago in outside hospital which showed munromicroabscess suggestive of psoriasis. He has been using medication for psoriasis since 1 month.
H/O unstable angina 1 and half year back-PTCA was done.
Not a K/C/O HTN,TB,asthma,epilepsy, thyroid disorders.
Personal history:
Diet-mixed
Appetite-normal
sleep-adequate
Bowel and bladder movements-regular
Family history:
Not significant
General examination:
Patient is conscious, coherent, cooperative.
No pallor,icterus,cyanosis,clubbing,lymphadenopathy,edema.
Vitals on admission:
Temperature-99 F
PR-64 bpm
RR-18 cpm
BP-80/60 mmHg
Systemic examination:
CVS-S1,S2 heard,No murmurs
CNS-No FND
P/A-soft,non tender
Clinical images:
Psoriatic plaques on B/L upper and lower lims:
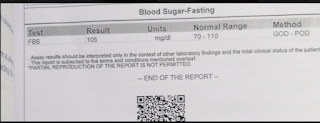
Investigations:
Provisional dignosis:
Fever under evaluation with myalgias under evaluation with low backache 2°to radiculopathy.
With H/O PTCA 1 and half year back
With K/C/O DM-type 2
Treatment:
IVF NS @150 ml/hr-bolus given
@75 ml/hr- maintenance
TAB.DOLO 650MG TID
INJ.NEOMOL 1G IV SOS
Temperature charting 4th hrly
INJ.AVIL 2CC SOS(IF CHILLS +)
GRBS monitoring 6th hrly
INJ.HUMAN ACTRAPID ACCORDING TO GRBS
TAB.ECOSPIRIN 75/20 MG PO OD
INJ.PIPTAZ 4G IV QID















Comments
Post a Comment